Benign Prostatic Hyperplasia (BPH) Treatment
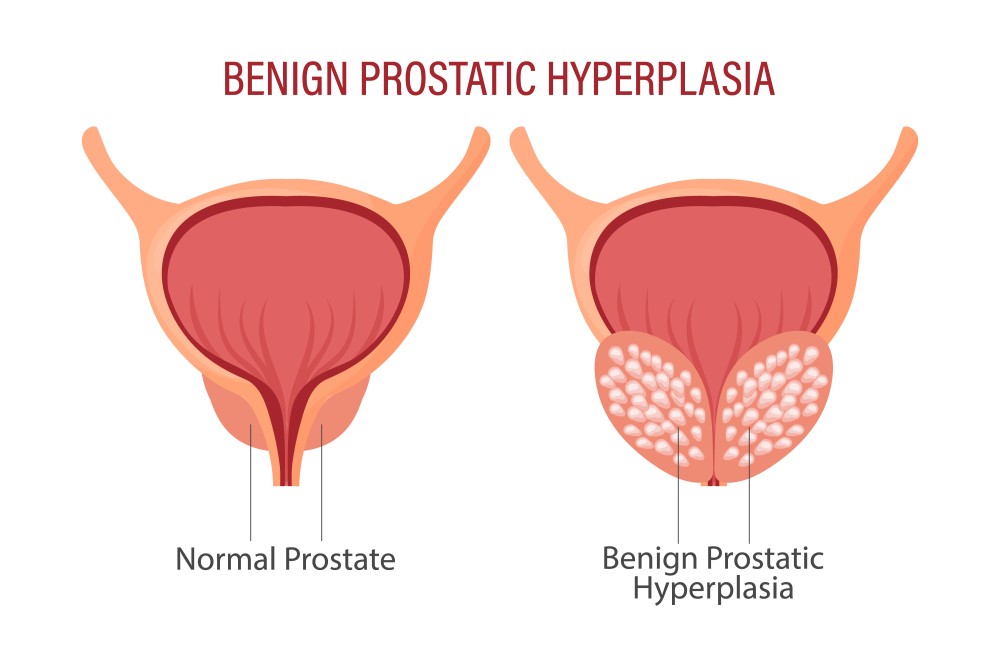
Benign Prostatic Hyperplasia (BPH) is a common condition in older men characterized by the non-cancerous enlargement of the prostate gland, which can cause urinary symptoms such as frequency, urgency, and obstruction. Treatment options for BPH aim to alleviate symptoms, improve quality of life, and manage any complications.
1. Lifestyle Modifications:
- Dietary Changes: Encourage a diet rich in fruits, vegetables, and whole grains. Reducing caffeine and alcohol intake can help minimize urinary symptoms.
- Fluid Management: Advise limiting fluid intake in the evening to reduce nighttime urinary frequency.
- Bladder Training: Implementing scheduled voiding and bladder training techniques can help manage symptoms.
2. Medications:
- Alpha-Blockers: These drugs (e.g., tamsulosin, alfuzosin) relax the smooth muscles of the prostate and bladder neck, improving urine flow and reducing symptoms. They work quickly but do not reduce prostate size.
- 5-Alpha-Reductase Inhibitors: Medications such as finasteride and dutasteride reduce the size of the prostate by inhibiting the conversion of testosterone to dihydrotestosterone (DHT). They may take several months to show effects and are often used in combination with alpha-blockers.
- Combination Therapy: In some cases, a combination of alpha-blockers and 5-alpha-reductase inhibitors is used for a more comprehensive approach to symptom management and prostate reduction.
- Anticholinergics: Used in cases with significant bladder outlet obstruction or overactive bladder symptoms, these medications help reduce bladder urgency and frequency.
3. Minimally Invasive Procedures:
- Transurethral Resection of the Prostate (TURP): A common surgical procedure where excess prostate tissue is removed using a resectoscope inserted through the urethra. It effectively relieves urinary obstruction and improves symptoms.
- Transurethral Incision of the Prostate (TUIP): Involves making small incisions in the prostate to relieve pressure on the urethra. This procedure is typically used for smaller prostates.
- Laser Therapy: Techniques like Holmium Laser Enucleation of the Prostate (HoLEP) or GreenLight laser therapy use lasers to remove or vaporize excess prostate tissue with precision.
- Prostatic Urethral Lift (PUL): A minimally invasive procedure where implants are placed to lift and hold the enlarged prostate tissue away from the urethra, improving urine flow.
4. Surgical Options:
- Open Prostatectomy: In cases of very large prostates or when other treatments are not effective, this procedure involves removing part or all of the prostate through an incision in the abdomen. It is more invasive and has a longer recovery time but may be necessary for severe cases.
5. Monitoring and Follow-Up:
- Regular Check-ups: Monitor the effectiveness of treatment and adjust management plans as needed. Regular evaluations help assess symptom control, potential side effects, and disease progression.
- Symptom Assessment: Use tools such as the International Prostate Symptom Score (IPSS) to evaluate symptom severity and treatment outcomes.
6. Patient Education:
- Understanding BPH: Educate patients about the nature of BPH, treatment options, and potential side effects.
- Self-Management: Provide guidance on lifestyle changes, symptom management techniques, and when to seek medical attention.
7. Addressing Complications:
- Management of Complications: Address any complications such as urinary tract infections, bladder stones, or acute urinary retention that may arise from BPH.
Effective management of BPH involves a combination of lifestyle changes, medical treatment, and, in some cases, surgical intervention. Tailoring the treatment approach to the individual’s symptoms, prostate size, and overall health is crucial for achieving the best outcomes.
